Understanding Diabetic Kidney Disease: Prevention, Management, and Hope
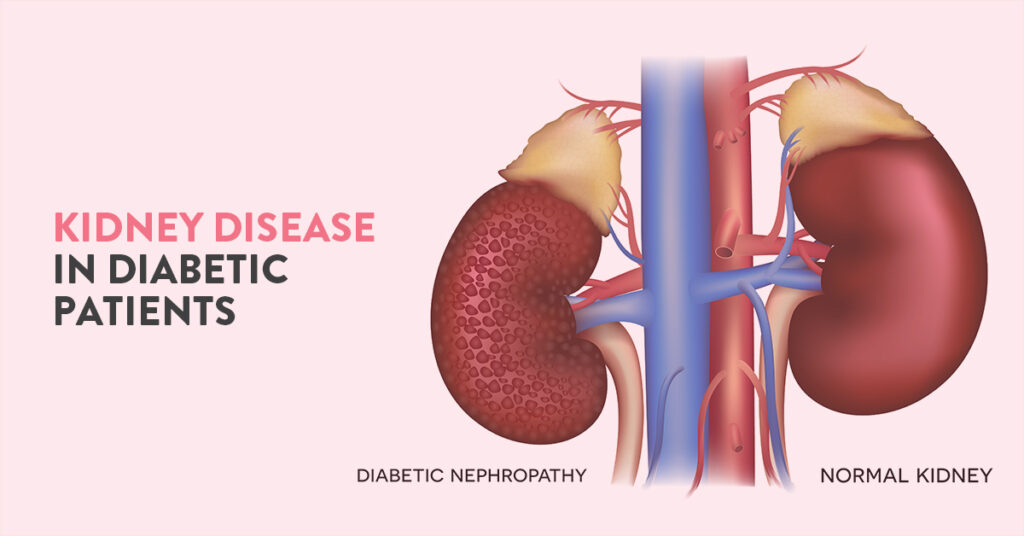
Diabetic kidney disease (DKD), also known as diabetic nephropathy, is one of the most significant complications of diabetes mellitus. Affecting nearly 20–40% of people with diabetes, DKD is a leading cause of chronic kidney disease (CKD) and end-stage kidney disease (ESKD) worldwide. Early recognition, proactive management, and adherence to preventive measures can drastically improve outcomes and quality of life for affected individuals.
What is Diabetic Kidney Disease?
DKD occurs when prolonged high blood sugar levels damage the small blood vessels (glomeruli) in the kidneys. These glomeruli filter waste products from the blood. Over time, this damage impairs the kidneys' ability to filter waste, leading to protein leakage (albuminuria) and progressive kidney dysfunction.
Risk Factors
- Uncontrolled blood sugar
- Hypertension
- Family history of kidney disease
- Smoking
- Obesity
- Duration of diabetes
Symptoms
Silent but Significant
In the early stages, DKD often remains asymptomatic, which underscores the importance of regular screenings. Symptoms of advanced DKD include:
- Swelling in the legs, ankles, or feet (edema)
- Fatigue
- Increased frequency or reduced output of urination
- Frothy urine (indicating protein leakage)
- Nausea or vomiting in later stages
Diagnosis
Routine testing for individuals with diabetes helps detect DKD early. Diagnostic tools include:
- Urine tests: To check for albuminuria or proteinuria
- Blood tests: To measure kidney function via estimated glomerular filtration rate (eGFR)
- Blood pressure monitoring: Since hypertension accelerates kidney damage
Prevention: The Cornerstone of DKD Management
Preventing DKD begins with optimal diabetes management and addressing associated risk factors:
- Tight Glycemic Control: Maintain HbA1c below 7% (or as individualized).
- Blood Pressure Management: Aim for <130/80 mmHg, using ACE inhibitors or ARBs if required.
- Regular Screenings: Annual kidney function tests, starting at diagnosis for type 2 diabetes or after 5 years for type 1 diabetes.
- Lifestyle Modifications:
- Quit smoking.
- Exercise regularly to maintain a healthy weight.
- Reduce salt intake and adopt a kidney-friendly diet.
Treatment: Slowing the Progression
Dr Neelesh Kapoor will decide on the best course of medications suited to your condition
Managing Comorbidities
- To treat hypertension, hyperlipidemia, and anemia to mitigate further kidney damage.
Emerging Therapies and Innovations
The field of nephrology is witnessing breakthroughs that offer hope to those with DKD:
- Precision Medicine: Personalized treatments based on genetic and molecular profiles.
- Artificial Intelligence in Nephrology: AI tools to predict DKD risk and progression.
- Kidney Regeneration Therapies: Stem cell and regenerative medicine approaches are under investigation.
Living with Diabetic Kidney Disease
DKD is not just a physical ailment; it also affects mental and emotional well-being. Psychological support and education are integral to empowering patients. Support groups, patient education programs, and access to multidisciplinary care can help manage the disease effectively.
Conclusion
Diabetic kidney disease is a serious complication, but it is not inevitable. Proactive management of diabetes, regular monitoring, and lifestyle modifications are key to prevention. For those diagnosed with DKD, advancements in treatment offer new hope. A collaborative approach involving healthcare providers, patients, and caregivers is crucial in managing DKD and improving outcomes.
When in doubt, reach out to us.